Time to get us all on the same page with a Diastasis Classification System. Adopting a more standard way of describing Diastasis Rectus Abdominis (DRA) gives us communication clarity and understanding across continuum of providers (docs-nurse practitioners-midwives-physios/PTs/OTs-fitpros), social media influencers, and the public.
Give it some thought.
To be clear, this proposed Diastasis classification system isn’t mine, but it is a starting point for all of us to consider. I actually appreciate that it is coming out of the Medical Doctor/Surgeon/Researcher space. They, the docs and NPs, are the starting place for so many on their pregnancy recovery journey, and they set the tone for patient beliefs and expectations around their Diastasis. As a clinician, I often find it hard to shift the perspective of a patient who has been told they need surgery for a DRA by their doctor. No matter the results we are achieving, their buy-in is trickier, and the work of conservative care seems pointless if surgery is the end result anyway.
The German Hernia Society and International Endohernia Society published a paper in 2019 (Reinpold et al) to suggested classifying a diastasis as Mild, Moderate, or Severe* based on an Inter-Recti Distance (IRD) width.
Mild (< 3 cm)
Moderate (3-5 cm)
Severe (> 5 cm)
While they were not specific as to the measurement point, they summarized multiple articles that used a variety of measurement points. These studies supported a consensus around a separation beyond 2 cm as a diastasis, including the 2009 study by Beer et al (Read more details about that here).
That seems too simple…
While this diastasis classification system may seem over-simplified, and I know I have regularly seen much larger Diastasis measures in my own practice, it is a communication starting point. It changes the gravity of social media posts and marketing of programs on how someone healed their own 3 cm DRA. How different would it be if…
- The same social media posts would now read-“find out how I healed my MILD Diastasis’
- A doctor suggested to a patient that the DRA was measuring as MILD, and therefore they are a great candidate for conservative care before considering another approach
- A new mama thinks- oh phew, my Diastasis is only MILD, I can do this!!
Helping to encourage folks to know their Diastasis baseline is also something I have written about before. The hill doesn’t seem so far to climb if you have a 3 or 4 cm IRD, and you know you started with a 2 cm naturally occurring separation pre-pregnancy. But if you think you started at zero, that takes your mindset to a very different place as you consider the information you are receiving.
But what about the fascia?!
I know what you are thinking- but what about the fascia?! We have moved forward to understanding more about the transmission of forces via the fascia, and the role it has in recovery challenges (no longer just looking at IRD). I AM ALL IN on that thought process and understanding it better. However, we still do not have a clinically accessible, and uniform way of describing and classifying fascia either. Real time ultrasound is awesome, but most clinicians are priced out.
After palpating A LOT of linea alba’s over the years, I know what density I’d like to feel, but my min/mod/max may not be the same as yours. And heads-up, you do not get an 8-12 cm IRD without some very thinned, low density fascia. They are part of the same clinical picture.
The reality is we need to be studying and quantifying the FUNCTION of the whole abdominal wall, and how to restore that. We are still sorting out the clinical meaning of a DRA at any width and fascial quality/density. So we have a long way to go. (Read more on one of my fave studies on abdominal wall function with and without DRA here).
In other words, IRD and fascial quality and density, still don’t paint the full clinical picture. Considering abdominal wall function, quality of life, and patient beliefs are more pieces of the puzzle we need to explore. So are genetics, but y’all….we can’t get it all into one blog! (I did put some other thoughts here)
Let’s reframe step-one.
The Reinhold study gives us a place to start. A Diastasis classification system to clarify our communication between providers, patients, and the public. I am not suggesting we move backward in our thought process (conflating IRD with DRA), however, meausring the IRD is objective, cost-effective, and still a primary tool used across specialties. It is also still the primary focus of the public. It may create an opportunity to use the classifications to advocate for patients who are not interested in surgery and can’t convince their doctors to write them a PT prescription. The Beer et al study suggestion of an IRD that is >2 cm at 3 cm above the navel has been utilized in a lot of research to distinguish what is and what is not a DRA. We can add this specific measurement location to the full scope of our intake paradigms. This can help to solidify that we are talking about the same thing when we talk across specialties about DRA.
The Reinpold article (free full text) also offered other classifications that do speak to fascia/connective tissue and other parameters that would help our communication among specialties including:
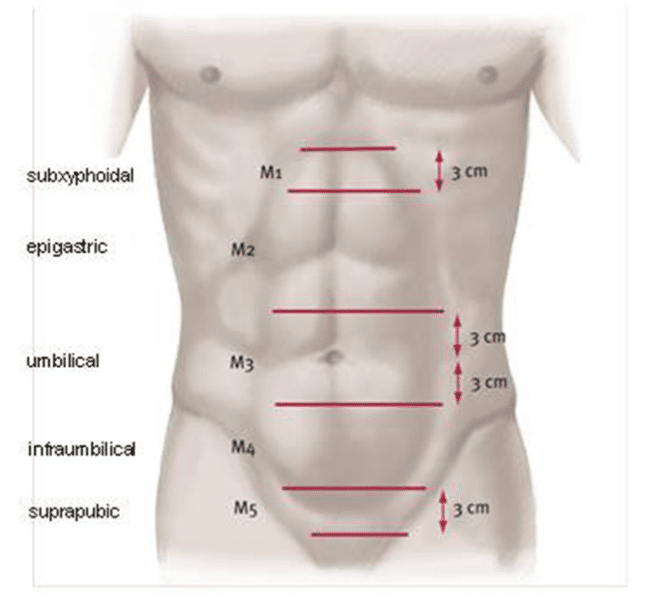
- DRA length and location of IRD- Subxiphoidal, Epigastric, Umbilical, Infraumbilical, and Suprapubic. (see picture)
- Number of previous pregnancies
- Skin laxity
- Clinical bulge while standing and with a sit-up
- (Picture Source- Reinpold et al 2019)
We have more work to do! Reframing step-one may be a really wise way to get us all heading in the same direction. Let me know what you think!
Don’t wanna miss a post and enjoy subscriber only content and discounts- join my newsletter here.
References:
Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A, Kukleta J, Kuthe A, Lorenz R and Stechemesser B (2019) Classification of Rectus Diastasis—A Proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front. Surg. 6:1. doi: 10.3389/fsurg.2019.00001.
*based on previous work- Ranney B. Diastasis recti and umbilical hernia causes, recognition and repair. SDJ Med. (1990) 43:5–8.
The Normal Width of the Linea Alba in Nulliparous Women. Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. Clin. Anat. 22:706–711, 2009.
2 thoughts on “A Diastasis Classification System”
I really like your argument that a uniform classification system would positively impact the client/patient perspective of their own DR. I completely agree! A more logistical question-Is there a certain device/brand you recommend for measuring IRD?
Hi there! I think it would help a lot both with communication and with protection of the public. I think the most uniformly accessible tool that can be objective is a tape measure. Simple, cheap, and no training required to use properly! Not perfect, but more consistent than fingers, and most folks have one in their drawers at the clinic.
Take it easy! Julie
This blog provides general information and discussion about medicine, health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician or other health care worker.
Never disregard professional medical advice or delay in seeking it because of something you have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or 911 immediately.